Actualidad

Publication 2024 |Visualization of the Intracranial Pressure and Time Burden in Childhood Brain Trauma
To validate the intracranial pressure (ICP) dose-response visualization plot for the first time in a novel prospectively collected pediatric traumatic brain injury (pTBI) data set from the multi-center, multi-national KidsBrainIT consortium.
Prospectively collected minute-by-minute ICP and mean arterial blood pressure time series of 104 pTBI patients were categorized in ICP intensity-duration episodes. These episodes were correlated with the 6-month Glasgow Outcome Score (GOS) and displayed in a color-coded ICP dose-response plot. The influence of cerebrovascular reactivity and cerebral perfusion pressure (CPP) were investigated. The generated ICP dose-response plot on the novel data set was similar to the previously published pediatric plot.
This study confirmed that higher ICP episodes were tolerated for a shorter duration of time, with an approximately exponential decay curve delineating the positive and negative association zones. ICP above 20 mm Hg for any duration in time was associated with poor outcome in our patients. Cerebrovascular reactivity state did not influence their respective transition curves above 10 mm Hg ICP. CPP below 50 mm Hg was not tolerated, regardless of ICP and duration, and was associated with worse outcome. The ICP dose-response plot was reproduced in a novel and independent pTBI data set. ICP above 20 mm Hg and CPP below 50 mm Hg for any duration in time were associated with worse outcome. This highlighted a pressing need to reduce pediatric ICP therapeutic thresholds used at the bedside.

Nuevo curso SmartCampus 2025 | Métodos diagnósticos para la evaluación de las alteraciones de la dinámica de LCR
La hidrocefalia es una de las patologías más frecuentes manejadas por los neurocirujanos. La hidrocefalia tiene múltiples etiologías y, en algunos casos, su fisiopatología es todavía controvertida. Paradójicamente, la patología más tratada en los servicios de neurocirugía carece todavía de una sistemática en el diagnóstico y en la justificación de las decisiones terapéuticas . Entre el arsenal diagnóstico del que dispone el neurocirujano, el registro de la presión intracraneal (PIC) y los diferentes tests para valorar la compliance y la dinámica del LCR son métodos todavía poco sistematizados, con importantes controversias en sus indicaciones y de interpretación no siempre fácil.
En este nuevo curso avanzado de SmartCampus (código: SC-H2-2025), pretendemos avanzar en la utilización de los estudios de la dinámica del LCR y en la monitorización de la PIC para optimizar el diagnóstico y la potencial selección de una determinada válvula en los adultos y niños con hidrocefalia y en los pacientes con alteraciones complejas de la dinámica del LCR (hidrocefalias tabicadas, quistes aracnoideos, etc.). Discutiremos a fondo la interpretación y la utilidad de los diferentes tests de dinámica de LCR que se utilizan con mayor frecuencia en el estudio de estos pacientes. También introduciremos técnicas de interpretación avanzada de los registros de PIC y clasificaremos los diferentes tipos de hidrocefalia en función de sus perfiles de PIC. Se presentarán diferentes opciones de software para monitorizar y analizar la PIC. En todos los módulos del curso, las presentaciones teóricas se complementarán con la presentación de casos prácticos que permitan consolidar los conocimientos adquiridos. Inscripciones: abiertas

Publication 2024 | Surgical Outcomes in Chiari 1 and Chiari 1.5 Malformation Treated by Posterior Fossa Reconstruction: A Comprehensive Analysis of 110 Pediatric Cases
The purpose of the current single-center study is to critically assess the one-year surgical outcomes of a cohort of 110 children with CM-1 or CM-1.5 who were treated using “posterior fossa reconstruction” (PFR), a surgical technique described in 1994 that has since been used in both adults and children. Methods:Patients included in this study were selected from a group of children with CMs who were operated on in our Pediatric Neurosurgical Unit between 1 January 2007 and 31 November 2023. Surgical outcome was defined based on clinical and neuroradiological results as very good, good, or bad. Results:The mean age of our child cohort was 9.9 ± 4.7 years, with 54 girls (49%) and 56 boys (51%). Sixty-six children had CM-1 (60%) while forty-four had CM-1.5 (40%). Following surgery, there was no neurological worsening or death among the children. Most children (70%) had an uneventful recovery and were discharged home on average one week after surgery. However, in 33 children (30%), we recorded at least one postoperative adverse event. The one-year surgical outcome was excellent in 101 children (91.9%), good in 5 (4.5%), and bad in 4 (3.6%). Conclusions: PFR significantly enlarges the volume of the posterior fossa and recreates a CSF environment that generates buoyancy of the cerebellum, with a high percentage of excellent and good clinical results evaluated one year post-surgery.

Nuevo curso SmartCampus 2025 | Actualizaciones y controversias en el paciente neurocrítico
La monitorización de la PIC es un método imprescindible para el manejo del paciente con patología neurológica aguda en riesgo de hipertensión intracraneal y por lo tanto en muchos pacientes neurocríticos (traumatismos craneales, hemorragia subaracnoidea espontánea, meningitis, etc.) . La razón fundamental que justifica el control de la PIC son las consecuencias letales de la hipertensión intracraneal. Numerosos trabajos han demostrado en las últimas tres décadas que la elevación de la PIC no es solo un indicador de la gravedad de la lesión y que, por lo tanto, debe controlarse dentro de unos límites, todavía imprecisos, pero que se acepta que deben ser inferiores a los 20 mmHg. Para los médicos intensivistas, neurocirujanos, neurólogos y personal de enfermería, la correcta comprensión de las causas y de los mecanismos que inducen la hipertensión intracraneal son imprescindibles para el correcto manejo de estos pacientes. En los últimos años, la discusión sobre temas aparentemente más avanzados (umbrales de presión, “dosis” de aumento de la PIC, manejo orientado a la PIC o a la PPC, PRx, autorregulación, etc.) han difuminado la actualización y comprensión de los conceptos básicos necesarios para entender la fisiopatología de la hipertensión intracraneal.
Esta cuarta edición del curso (código: SC-NCri2-2025) nueva edición del curso, diseñado de forma modular (cuatro módulos y 4 webinars), pretende ser una curso avanzado sobre conceptos que deberían ser bien conocidos por todos los implicados en el manejo de estos pacientes y que, sin embargo, por diversas razones, han pasado a ocupar un segundo lugar en los currículos de las diferentes especialidades. Esperamos que este nuevo curso sea de vuestro interés y cumpla con las expectativas manifestadas por los asistentes de anteriores ediciones de este curso integrado en el itinerario formativo dirigido al manejo del paciente neurocrítico .

Spanish translation of the posttraumatic stress disorder checklist | New publication!
The present study translated the PTSD Checklist for DSM-5 to Spanish and validated it in a sample of patients with TBI 6 months after the injury. Methods: The study included 233 patients (162 males and 71 females) recruited from four Spanish hospitals within 24 h of traumatic brain injury. Results: The analysis confirmed the internal consistency of the translated instrument (α = 0.95). The concurrent validity of the instrument was confirmed based on high correlation coefficients of 0.7 and 0.74 with the General Anxiety Disorder-7 (GAD-7) and Patient Health Questionnaire (PHQ-9), respectively. Conclusion: Overall, the results suggest that the Spanish translation of the PCL-5 is a reliable and valid instrument for screening PTSD symptoms among Spanish TBI patients. The Spanish translation of the PCL-5 is also presented in the manuscript.

Intracranial Pressure and Time Burden in Childhood Brain Trauma | New publication!
Prospectively collected minute-by-minute ICP and mean arterial blood pressure time series of 104 TBI children were categorized in ICP intensity-duration episodes. These episodes were correlated with the 6-month Glasgow Outcome Score (GOS) and displayed in a color-coded ICP dose-response plot. The influence of cerebrovascular reactivity and cerebral perfusion pressure (CPP) were investigated. The generated ICP dose-response plot on the novel data set was similar to the previously published pediatric plot. This study confirmed that higher ICP episodes were tolerated for a shorter duration of time, with an approximately exponential decay curve delineating the positive and negative association zones. ICP above 20 mm Hg for any duration in time was associated with poor outcome in our patients. Cerebrovascular reactivity state did not influence their respective transition curves above 10 mm Hg ICP. CPP below 50 mm Hg was not tolerated, regardless of ICP and duration, and was associated with worse outcome. The ICP dose-response plot was reproduced in a novel and independent data set. ICP above 20 mm Hg and CPP below 50 mm Hg for any duration in time were associated with worse outcome. This highlighted a pressing need to reduce pediatric ICP therapeutic thresholds used at the bedside.

Biomarkers in predicting CT scan results and neurological outcomes in children with traumatic brain injury | New publication!
In light of the burden of traumatic brain injury (TBI) in children and the excessive number of unnecessary CT scans still being performed, new strategies are needed to limit their use while minimising the risk of delayed diagnosis of intracranial lesions (ICLs). Identifying children at higher risk of poor outcomes would enable them to be better monitored. The use of the blood-based brain biomarkers glial fibrillar acidic protein (GFAP) and ubiquitin carboxy-terminal hydrolase-L1 (UCH-L1) could help clinicians in this decision. The overall aim of this study is to provide new knowledge regarding GFAP and UCH-L1 in order to improve TBI management in the paediatric population.

Glioblastoma Pseudoprogression Discrimination Using Multiparametric Magnetic Resonance Imaging | New Publication!
Pseudoprogression in glioblastoma presents a common challenge during clinical follow-up, significantly impacting disease management. In this study, the potential of multiparametric magnetic resonance imaging (MRI) alongside principal component analysis and advanced machine learning techniques was explored to distinguish pseudoprogression from true tumor progression. This study, conducted in the extended neurosurgery service of both Vall d'Hebron and Arnau de Vilanova University Hospitals, sheds light on the ability of multiparametric MRI combined with analysis and machine learning techniques to enhance discrimination between glioblastoma pseudoprogression and true tumor progression. The findings offer valuable insights to optimize diagnostic approaches and improve clinical management of this devastating disease.

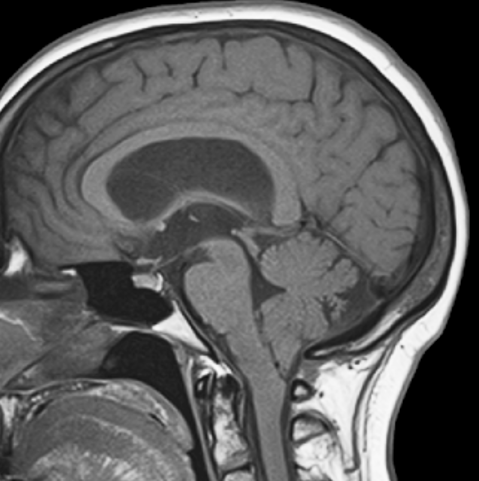
A Critical Update of the Classification of Chiari and Chiari-like Malformations | New Publication!
Chiari malformations are a group of craniovertebral junction anomalies characterized by the herniation of cerebellar tonsils below the foramen magnum, often accompanied by brainstem descent.
This review aims to examine the various classification approaches employed and proposes a simplified scheme to differentiate between different types of tonsillar herniations. Furthermore, it explores the most appropriate terminology for acquired herniation of cerebellar tonsils and other secondary Chiari-like malformations. Recent advances in magnetic resonance imaging (MRI) have revealed a higher prevalence and incidence of Chiari malformation Type 1 and identified similar cerebellar herniations in individuals unrelated to the classic phenotypes described by Chiari. As we reassess the existing classifications, it becomes crucial to establish a terminology that accurately reflects the diverse presentations and underlying causes of these conditions.
This paper contributes to the ongoing discussion by offering insights into the evolving understanding of Chiari malformations and proposing a simplified classification and terminology system to enhance diagnosis and management.
Proyecto investigación Chiari | Concesión beca FIS
En la última convocatoria de Becas FIS resuelta en diciembre de 2022 nuestra unidad ha recibido financiación para desarrolar en los próximos tres años el proyecto "Impacto del síndrome afectivo-cognitivo cerebeloso (Síndrome de Schmahmann) en los pacientes con una malformación de Chiari tipo 1" (PI22/01082) .
En la actualidad se acepta que el cerebelo participa como un modulador de funciones cognitivas como la atención, la memoria, el lenguaje, capacidades visuoconstructivas, funciones ejecutivas y en el afecto y las emociones. El denominado síndrome afectivo-cognitivo cerebeloso descrito en 1998 se caracteriza por déficits en las funciones ejecutivas, en el procesamiento lingüístico, en la cognición espacial y en la regulación afectiva. Nuestro estudio pretende determinar la repercusión de la malformacion de Chiari 1 y 1.5 en la cognición, la regulación afectiva, la personalidad y su impacto en la calidad de vida de estos pacientes. Relevancia: Se pretende que este estudio permita verificar/refutar la existencia de este síndrome en los pacientes con una malformación de Chiari y su perfil cognitivo-afectivo. Esto permitirá, diseñar en un futuro utilizar una herramienta de evaluación adecuada como la escala de Schmahmann para el cribaje de estos pacientes, objetivar las dificultades neuropsicológicas que presentan y programar intervenciones personalizadas dirigidas a mejorarlas.

Post-Doctoral Research position
VHIR offers a postdoctoral position within the Unidad de Investigación de Neurotraumatologia y Neurocirugia (UNINN). The candidate will participate in projects focused on the basic and clinical research on traumatic brain injury, brain edema and hydrocephalus.
Main responsibilities and duties:1. Project Management; 2. Project Applications; 3. Writing scientific reports and papers; 4. Attending projects meetings and scientific conferences and 5. Support PhD researchers. Required qualifications: 1. Ph.D. degree with a strong research background in neurobiology within the past 5 years; 2. Bench work experience is required; 3. Proactive, dynamic, and outstanding organizational skills; 4. Good communication skills and fluency in spoken and written English (minimum level in English: C); 5. Experience on international project management and project applications and 6. A demonstrated ability to work in a multidisciplinary and diverse team.
Perceived Utility of Intracranial Pressure Monitoring in Traumatic Brain Injury | New publication!
OBJECTIVE:To study the monitoring practices of an established expert panel (the clinical working group from the Seattle International Brain Injury Consensus Conference effort) to examine the match between monitoring guidelines and their clinical decision-making and offer guidance for clinicians considering monitor insertion. METHODS: We polled the 42 Seattle International Brain Injury Consensus Conference panel members' ICP monitoring decisions for virtual patients, using matrices of presenting signs (Glasgow Coma Scale [GCS] total or GCS motor, pupillary examination, and computed tomography diagnosis). Monitor insertion decisions were yes, no, or unsure (traffic light approach). We analyzed their responses for weighting of the presenting signs in decision-making using univariate regression.
CONCLUSION: Candidacy for ICP monitoring exceeds published indicators for monitor insertion, suggesting the clinical perception that the value of ICP data is greater than simply detecting and monitoring severe intracranial hypertension. Monitor insertion heatmaps are offered as potential guidance for ICP monitor insertion and to stimulate research into what actually drives monitor insertion in unconstrained, real-world conditions.
Noninvasive evaluation of hyperventilation therapy | New UNINN publication!
The ICFO together with the UNINN have published in the J. Neurotrauma a paper dedicated to non-invasive monitoring of hyperventilation in patients with TBI. Hyperventilation (HV) therapy uses vasoconstriction to reduce intracranial pressure (ICP) by reducing cerebral blood volume. However, as HV also lowers cerebral blood flow (CBF), it may provoke misery perfusion (MP) where the decrease in CBF is coupled with increased oxygen extraction fraction (OEF). MP may rapidly lead to the exhaustion of brain energy metabolites, making it vulnerable to ischemia.. Our study provides pilot data demonstrating that bedside transcranial hybrid near-infrared spectroscopies could be utilized to assess potential misery perfusion.

PhD student position
VHIR offers the possibility of a collaboration with the Unidad de Investigación de Neurotraumatologia y Neurocirugia (UNINN) . The candidate will participate in projects focused on the study of cognitive alterations secondary to traumatic brain injury, hydrocephalus, and in the study of the cerebellar cognitive-affective syndrome in patients with Chiari 1 malformations.
Requirement for applying to the position are: 1. Degree in Psychology ; 2. Official Master general sanitario; 3. At the time of submitting the application, not to be in possession of any doctoral degree, nor have enjoyed more than 12 months of any other specific contract for pre-doctoral research staff in training;4. Commitment to register the doctoral thesis in the next available period (September 2023).

Diagnosis and Treatment of Normal-Pressure Hydrocephalus Syndrome | New Publication!
We have collaborated as guest editors in the special issue on Diagnosis and Treatment of Normal-Pressure hdrocephalus Syndrome This focused issue has been completed and published in the Clinical Neurology section of the Jourrnal of Clinical Medicine (IF: 4.96).
In this focused issue, ten papers have been published that review many controversial aspects regarding the screening methods, diagnostic tests, and treatment of patients with NPH that are relevant to individualizing treatment and improving outcomes after surgery. Three of the 10 published papers come from the Vall d'Hebron University Hospital's neurosurgery department. One of our major contributions has been a thorough analysis of the many kinds of devices that can be used to shunt patients with NPH. We stress the need of the neurosurgeon being knowledgeable about the variations among commercially available devices and avoiding the usual error of selecting a one-size-fits-all system for this particular patient population. We emphasize the need for the neurosurgeon to be aware of the differences among commercially-available devices and to avoid the common mistake of choosing a one-size-fits-all system for this group of patients. The variables to take into account for selecting the most appropiate CSF device are discussed. We believe that a more rational approach to shunting increases the chances of a positive outcome and increase the quality of life of patients with this syndrome.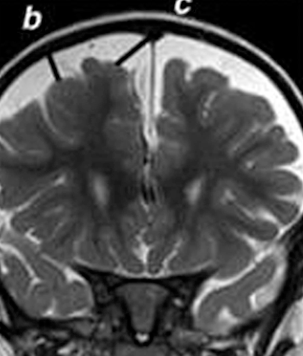
Non-invasive diagnostic of benign external hydrocephalus in kids | New UNINN publication!
Benign external hydrocephalus (BEH) is considered a self-limiting pathology with a good prognosis. However, some children present a pathological intracranial pressure (ICP) characterized by quantitative and qualitative alterations (the so-called B-waves) that can lead to neurological sequelae.
We recruited eleven patients (median age 16 months, range 7 to 55 months) with BEH and an unfavorable evolution requiring ICP monitoring. Bedside, nocturnal monitoring using near-infrared time-resolved and diffuse correlation spectroscopies synchronized to the clinical monitoring was performed. We were able to detect noninvasively StO2 and BFI variations —with optical techniques in BEH children. This new technique helps in managing children with BEH.

Cochrane Injuries Group
We are pleased to share the news that one of the members of our Research Unit (J. Sahuquillo, Department of Neurosurgery, Vall d’Hebron University Hospital) has recently joined the Cochrane Injuries group as a Clinical editor.
The Cochrane Injuries group is part of the Cochrane Collaboration, an international not-for-profit and independent organisation, dedicated to making up-to-date, accurate information about the effects of healthcare. The work involves preparing, maintaining and promoting systematic reviews for the prevention, treatment and rehabilitation of traumatic injury, including the emergency resuscitation of seriously injured and burned patients. 
Secondary Analysis of the RESCUEicp Randomized Clinical Trial | Publicación UNINN
Our unit collaborated actively in the design and implementation of the multicenter multinational RESCUEicp clinical trial about the use of decompressive craniotomy in the management of patients with raised intracranial pressure which results were published in 2016. The secondary analysis of the RESCUEicp have been published on June 6, 2022 to explore the 24-month outcomes for patients with traumatic intracranial hypertension who receive a decompressive craniectomy. Findings: In this prespecified secondary analysis of a randomized clinical trial, 408 adults received either decompressive craniectomy or standard care. The Extended Glasgow Outcome Scale was used to assess 24-month outcomes in this secondary analysis; surgical patients had sustained reduced mortality but higher rates of vegetative state, severe disability, and moderate disability at 24 months.
Conclusions and Relevance.At 24 months, patients with surgically treated posttraumatic refractory intracranial hypertension had a sustained reduction in mortality and higher rates of vegetative state, severe disability, and moderate disability. Patients in the surgical group were more likely to improve over time vs patients in the medical group.
Publicación UNINN | Conferencia Consenso Chiari en Adultos | Neurological Sciences
El servicio de Neurocirugía del Hospital Universitario Vall d'Hebron ha participado en la publicación de las primeras recomendaciones internacionales para el diagnóstico y tratamiento de la malformación de Chiari tipo 1 en el adulto. Las malformaciones de la charnela craneocervical son una de las líneas de investigación traslacional consolidadas de la UNINN.
Un panel multidisciplinar de expertos elaboraron un documento de consenso. Después de una revisión basada en la evidencia y debates posteriores, se formularon 63 declaraciones agrupadas en 4 dominios (definición y clasificación/planificación/cirugía/siringomielia).El documento de consenso introduce 63 recomendaciones de expertos dirigidas a médicos e investigadores que tratan a adultos con Chiari y siringomielia.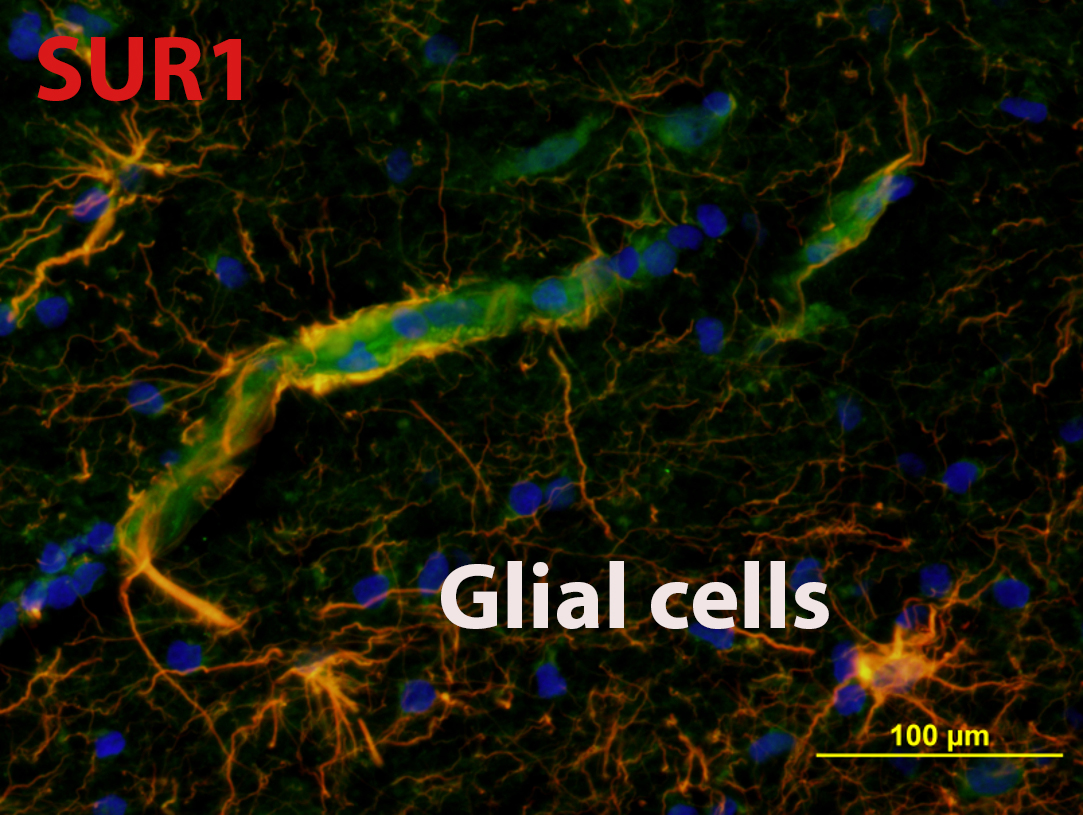
Sulfonylurea Receptor 1 in Central Nervous System Injury | Publicación UNINN
In the last few years, our research unit has focused on the study of Sulfonylurea receptor 1 (SUR1) as a target receptor for the management of postraumatic brain edema. In this focused review Jha et al. update the role of SUR1 in CNS injuries and their treatment.

Conferencia Consenso Chiari en Pacientes pediátricos | Publicación | Neurological Sciences
El servicio de Neurocirugía del Hospital Universitario Vall d'Hebron ha participado en esta segunda publicación de las recomendaciones internacionales para el Diagnóstico y Tratamiento de la malformación de Chiari tipo 1 en pacientes en edad pediátrica. Las malformaciones de la charnela craneocervical son una de las líneas de investigación traslacional consolidadas de la UNINN.Chiari malformation type 1 (CM1) is a rare condition where agreed classification and treatment are still missing. The goal of this study is to achieve a consensus on the diagnosis and treatment of CM1 in children.
The consensus document consists of 58 statements (24 on diagnosis, 34 on treatment), serving clinicians and researchers following children with CM1. There is a clear need for establishing an international network and registry and to promote collaborative studies to increase the evidence base and optimize the long-term care of this patient population.
Neurodevelopmental profile in children with benign external hydrocephalus syndrome | Publicación UNINN
New! The management of children with benign external hydrocephalus (BEH) remains controversial. Most BEH children do well in the long-term, but a substantial number have temporary or permanent psychomotor delays. The study aims to assess the prevalence and pattern of neurodevelopmental delay in a cohort of children with BEH. Results: Eighteen children (43%) presented statistically lower scores in the gross motor and composite motor of the Bayley-III scales compared to their healthy peers. Conclusion: In BEH, it is important to establish a diagnostic algorithm that helps to discriminate BEH patients that have self-limiting delays from those at risk of a persistent delay that should be referred for additional studies and/or interventions that might improve the natural evolution of a disease with high impact on the children and adult’s quality of life.
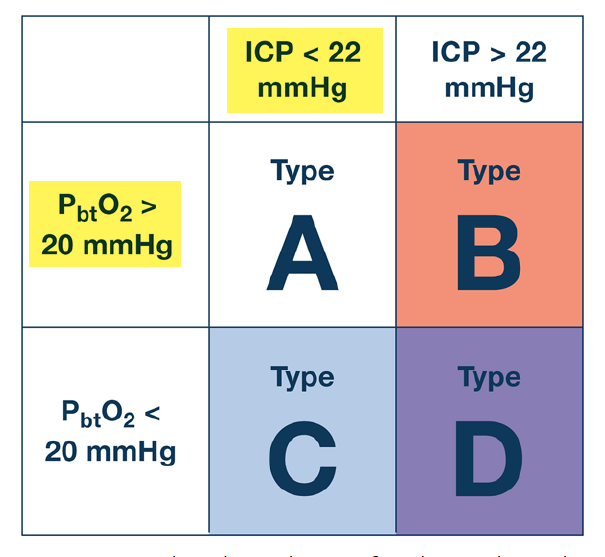
A management algorithm for adult patients with both brain oxygen and intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC) | Publicación UNINN
Current guidelines for the treatment of adult severe traumatic brain injury (sTBI) consist of high-quality evidence reports, but they are no longer accompanied by management protocols. We aimed to establish a modern sTBI protocol for adult patients with both intracranial pressure (ICP) and brain oxygen monitors in place.
Our consensus working group consisted of 42 experienced and actively practicing sTBI opinion leaders from six continents. We established three distinct treatment protocols, each with three tiers whereby higher tiers involve therapies with higher risk. One protocol addresses the management of ICP elevation when brain oxygenation is normal. A second addresses management of brain hypoxia with normal ICP. The third protocol addresses the situation when both intracranial hypertension and brain hypoxia are present.
These protocols should be used in conjunction with recommendations for basic care, management of critical neuroworsening and weaning treatment recently published in conjunction with the Seattle International Brain Injury Consensus Conference.
Management algorithm for patients with intracranial pressure monitoring: the Seattle International Severe Traumatic Brain Injury Consensus Conference (SIBICC) | Publicación UNINN
We provide comprehensive algorithms for ICP-monitor-based adult sTBI management. Consensus established 18 interventions as fundamental and ten treatments not to be used. We provide a three-tier algorithm for treating elevated ICP. Treatments within a tier are considered empirically equivalent. Higher tiers involve higher risk therapies. Tiers 1, 2, and 3 include 10, 4, and 3 interventions, respectively. We include inter-tier considerations, and recommendations for critical neuroworsening to assist the recognition and treatment of declining patients. Novel elements include guidance for autoregulation-based ICP treatment based on MAP Challenge results, and two heatmaps to guide (1) ICP-monitor removal and (2) consideration of sedation holidays for neurological examination.






